The Challenge
Access to care is an essential component of healthcare quality. It follows that ensuring access to care is one of the priorities emphasized by the Centers for Medicare and Medicaid Services (CMS) as part of its mission to ensure that Medicare beneficiaries receive consistently high-quality care. When the COVID-19 pandemic led to the declaration of a public health emergency in March 2020, utilization of the healthcare system for routine matters such as annual well visits and screenings declined, which many feared would lead to a subsequent spike in serious, preventable illnesses.
The IPRO QIN-QIO responded by offering healthcare providers education and resources to support their efforts to encourage patients to obtain routine and preventative care during the pandemic. Using the Medicare-covered Annual Wellness Visit as a proxy measurement for access to care, one Delaware-based medical group was able to record a measurable improvement in this area by deploying a range of specific strategies.
Background
Rarely have there been events that so clearly demarcate time as the emergence of COVID-19 and the declaration of a public health emergency in March 2020. One of the most noticeable and measurable effects of the pandemic was the sharp decline in health care utilization as consumers avoided hospitals and many outpatient practices temporarily closed in March and April 2020. A June 2020 survey of nearly 5,000 adults found that more than 40 percent reported having delayed or avoided medical care, including urgent and emergent care, due to the pandemic. (Mark É. Czeisler, Kristy Marynak and Kristie E.N. Clarke)
It took some time before community-based practices and patients were comfortable using telehealth as a substitute for in-person visits. By August 2020, the Journal of Public Health declared, “Broadband Internet Access is a Social Determinant of Health!” (Natalie C. Benda PhD). Not only were those without internet access prevented from participating in telehealth visits, but they were also made more vulnerable by the lack of access to credible information.
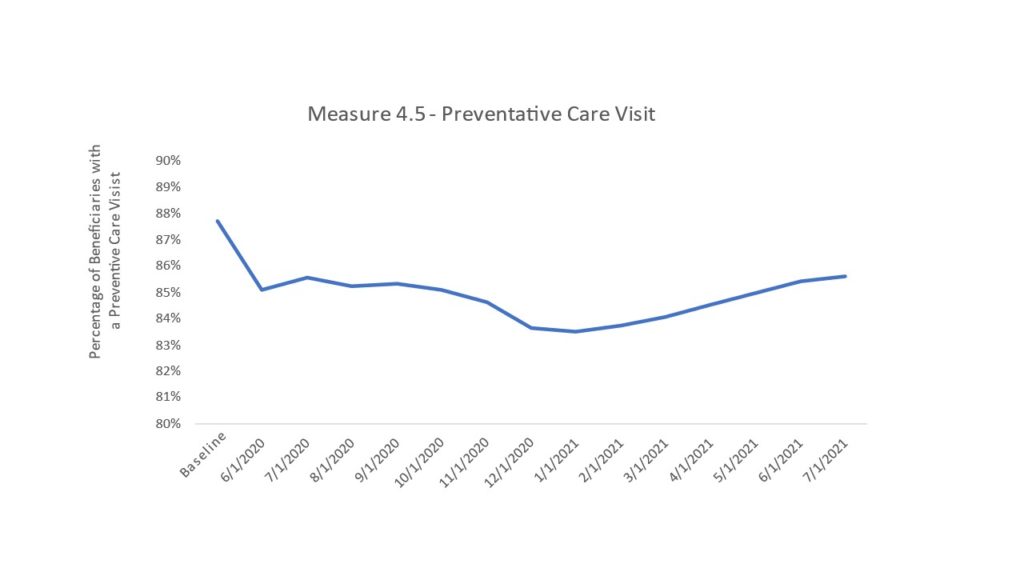
Several studies have explored the decreases in utilization, noting that outpatient visits, healthcare screenings, and elective surgeries saw steep declines. (The Commonwealth Fund) These findings are consistent with our own analysis (see Table 1), which shows a significant decline in prevention and wellness visits from baseline (Q4 2019) with a slow but steady increase since January 2021.
Action Steps
Using Annual Wellness Visit as a proxy measure for access to care, the IPRO QIN-QIO noted that prior to the pandemic, the vast majority of these visits were conducted in person. With the emergence of telehealth and several significant changes to Medicare which supported its use, including the ability for providers to conduct the AWV using audio only; the acceptance of patient-reported weight and blood pressure, and reimbursement for telehealth visits that equaled rates for in-person visits, the AWV could more easily be provided remotely.
Community-based providers would have to quickly pivot in order to successfully transition to telehealth. IPRO supported them by offering the following educational opportunities:
- A special six-week ECHO, Expanded Telehealth Services for COVID-19: Making Sense of the New Rules, offered in partnership with the Rhode Island Geriatric Education Center
- Medicare Telehealth and Remote Patient Monitoring (RPM) Services Guide, developed with experts from the Northeast Telehealth Resource Center
- Telehealth Practice Innovations During the COVID-19 Pandemic Webinar Series, a five-month Learning and Action Network (LAN) offered to Community Coalitions and recruited nursing homes
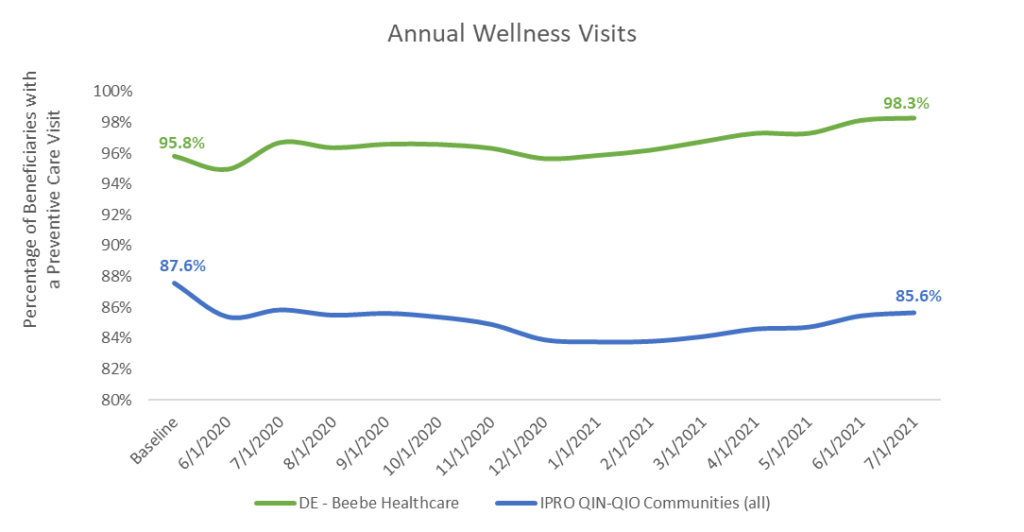
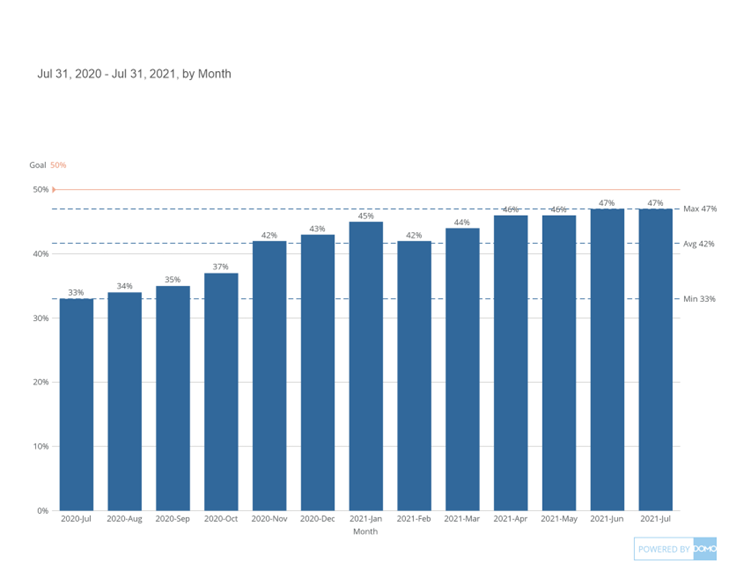
From baseline levels recorded prior to the COVID-19 pandemic through July 2021, of the 86 Community Coalitions that are part of the IPRO QIN-QIO, only three recorded improvements in their AWV completions. Of those three, only one met the CMS measure. This Community Coalition, anchored by Beebe Healthcare, a health system in southern Delaware, deployed specific strategies that leveraged communication, education and data to improve patient engagement.
Strategies for Success
Once the stay-at-home order was lifted on June 1, 2020, Beebe Healthcare Medical Group activated its plan to increase preventative care. It included:
- Revamping scheduling templates to include designated AWV slots which allowed for AWV times to be
- Easier to identify
- Protected from being booked by other types of appointments
- Available for other work groups to schedule
- Training of other collaborative work groups to schedule in the EMR including
- Population health
- ACO
- Primary Care Referral Line
- Internal dedicated staff
- Educating providers and team members on the value of wellness visits via
- Primary Care Meetings every Tuesday
- Monthly Provider Meetings
- Personal, live, telephone calls and outreach specifically to patients whose AWV appointments were due
- Dedicated staff in office making calls
- Reports on specific patients with AWV’s due run monthly and refreshed to include newly due patients
- Offering a variety of ways for patients to be seen as soon as possible
- By provider in person
- Remotely via telemedicine
- In person nurse visits
- Incentivizing providers by posting met goals and an AWV “leader list” every week at the Tuesday Primary Care Meetings
- Encouraging providers to combine visits and allowing add-on visits for AWVs
The Results
Beebe Healthcare Medical Group achieved a significantly higher rate of AWV completions than 85 other communities across the IPRO QIN-QIO region of 11 states and the District of Columbia (see Table 2).
“Adopting and modeling a patient centered medical home has assisted our team in driving patient centered outcomes. We value the importance of educating our patients on preventative health for better outcomes. The annual wellness visit is not treated as a physical exam. It is a conversation between a patient and their care provider to discuss their health and areas of concern in the future. We utilize the time to discuss their behavioral health, social factors, and family history in addition to clinical care,” said Danielle Socrates, Director of Performance Operations at Beebe Healthcare. “Creating templates and protecting scheduled time for patients to be seen in the office for annual wellness visits has also allowed us an opportunity to discuss preventive measures like flu shots and other vaccines, to assist in closing gaps in care.”
Works Cited
Mark É. Czeisler, et al. Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns — United States, June 2020. 11 September 2020. 12 May 2022.
Natalie C. Benda PhD, Tiffany C. Veinot PhD, MLS, Cynthia J. Sieck PhD, MPH, and Jessica S. Ancker PhD, MPH. AJPH. 8 July 2020. 12 May 2022.
The Commonwealth Fund. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits. 19 May 2020. 12 May 2022.